Type 1 diabetes is an autoimmune disease that leads to destruction of pancreatic islet cells. For many years, islet transplantation has been the focus of intense investigation as an insulin replacement therapy. Although transplantation immediately achieves insulin independence, the natural ability to continue producing insulin all but disappears 5 years later.
There are many problems with transplanting islet cells: A lack of donor tissue, limited numbers of islets per patient, and damage during isolation resulting in apoptosis and heightened immunogenicity. Recipients of transplanted cells require lifelong immunosuppression to prevent rejection.
Islet cells in vivo are surrounded by an extracellular matrix, which forms a unique microenvironment, or niche that provides the critical architectural, biochemical, and physical cues for maintaining the cells’ function. Studies using a variety of synthetic materials have shown improved beta-cell survival. It would be ideal if an authentic pancreatic niche could be replicated in vitro.
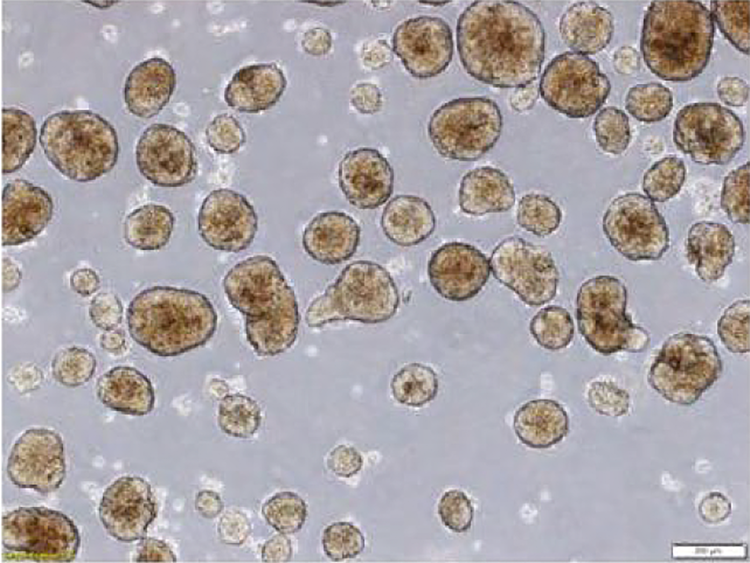
Dr. Xiao-Deng Chen is the lead author of a new article describing the results of an experiment in which a novel extracellular matrix culture system was designed and used in culturing islet cells. The matrix was successful in mimicking the pancreatic niche. It promoted islet cell attachment, growth, and function in tissue culture procedures. The matrix also restored the islet cells basement membrane which is evident in reducing immunogenicity. Performing islet cells isolation and expansion with this culture system supports allograft transplantation as a viable therapy for treating type 1 diabetes.
Dr. Xiao Dong Chen M.D, Ph.D., is a tenured professor at UT Health San Antonio. Dr. Chen also serves as the Chief Scientific officer of StemBioSys. The novel extracellular matrix described is available to investigators as CELLvo™ Matrix.
Caltag Medsystems are the European distributor for StemBioSys – contact techsupport@caltagmedsystems.co.uk for further information about the products.
